Department Introduction
Orthopedics | Excellence
:::



Department Introduction
Excellence
The third eye! Using the robotic arm for artificial joint replacement will only create small wounds for fast recovery.
The robotic arm is opening a new era of orthopedic treatment! The navigation system is conducive to the implementation of accurate surgery~


Professor Horng-Chaung Hsu
The robotic arm is like "the third eye and the third hand" of the orthopedist. Orthopedic surgeons say that for the artificial knee replacement surgery in Taiwan, the introduction of the robotic arm for replacement of artificial knee joint will not only help improve the accuracy of operation but also make the wound smaller and allow recovery at a faster pace. The past experience has found that with the help of the robotic arm, the recovery time after surgery can be shortened effectively and the patients can enjoy better quality of life!
In the past, when it came to the orthopedic surgery, most people would hold that the surgery time would be long, it would require a longer period for recovery, and the wound would be larger with more bleeding. However, Dr. Hsu Hung-chang as the director of the Department of Orthopedics in the China Medical University Hospital, says that with the advancement of medical technologies, the new type of robotic arm for replacement of the artificial knee joint has made great improvements to the above-mentioned problems.

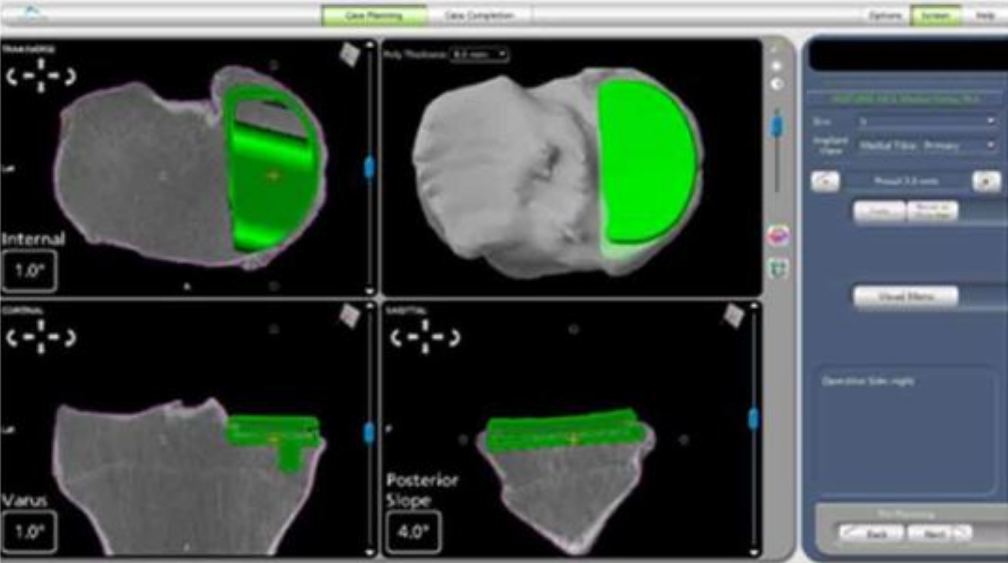
According to research, the failure rate of the surgery with the robotic arm can be reduced to 1/10 of that of the traditional surgery and the precision rate can be improved by 3 to 4 times. Director Horng-Chaung Hsu points out that robotic arm surgery will have to implement the 3D computerized tomography scanning on the affected parts (from the hip joint to the ankle) in the preoperative stage, and then the data need to be transferred to the robotic arm for preoperative planning and intraoperative implementation. Physicians can make visual and tactile interactions with the computer inside the robotic arm while the operation is in progress and adjust the patient's ideal positions at any time (either statically or dynamically), thus helping improve the accuracy of the operation.
Moreover, this surgical method is also superior to the computerized navigation surgery, since computerized navigation can only guide you on how to do it, and it is beyond the control in terms of "execution." Therefore, it is still possible to create an "exceptional" situation. However, the robotic arm is different. With the help of the above visual and tactile interactions, more effective and accurate implementation can be ensured. In addition, the robotic arm can accurately locate the characteristics of the surgery process, and more effectively help reduce the destruction of the knee during the surgery by trying to keep the patient's original knee, which reduces postoperative scar tissues and shortens the recovery period.

Most importantly, compared with the traditional total knee arthroplasty in the past, it can further reduce the need for postoperative patients to "learn" and "adapt" or even "change" their original kinematics, and effectively improve patient operation Satisfaction, so that their daily activities or sports almost restored as ever.
According to research, the technology for accurate replacement of the medial artificial knee joint will also improve the patient's tarsal femoral joint stability and reduce the extent of further deterioration. Precise replacement of the lateral artificial knee can also improve the stability of the medial femoral tibia and the joint space. Thus, precise placement of artificial partial knee joint can slow down the emergence of degenerative arthritis in other bone joints owing to one part, thus preventing the disease from entering into a vicious circle.

Figure 1. A woman surnamed Wu had a traditional surgery on the left knee and a robotic arm surgery on the right knee. The robotic arm surgery for joint replacement only creates a smaller wound and the recovery period is shortened as well.
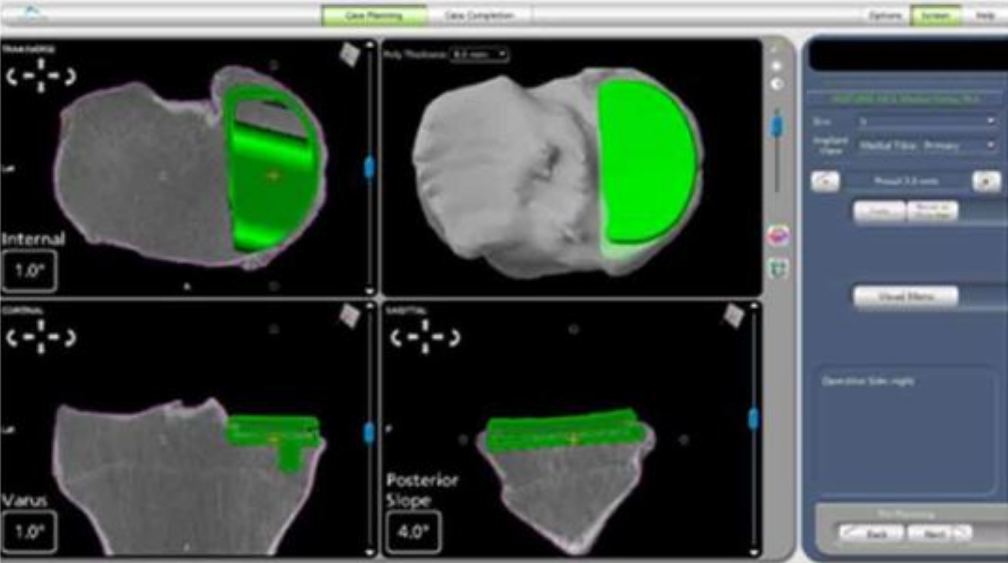
Figure 2. The robotic arm surgery requires 3D computed tomography scanning of the affected parts (from the hip joint to the ankle joint) to be performed prior to surgery. Then, the data will be transferred to the robotic arm for preoperative planning and intraoperative implementation.
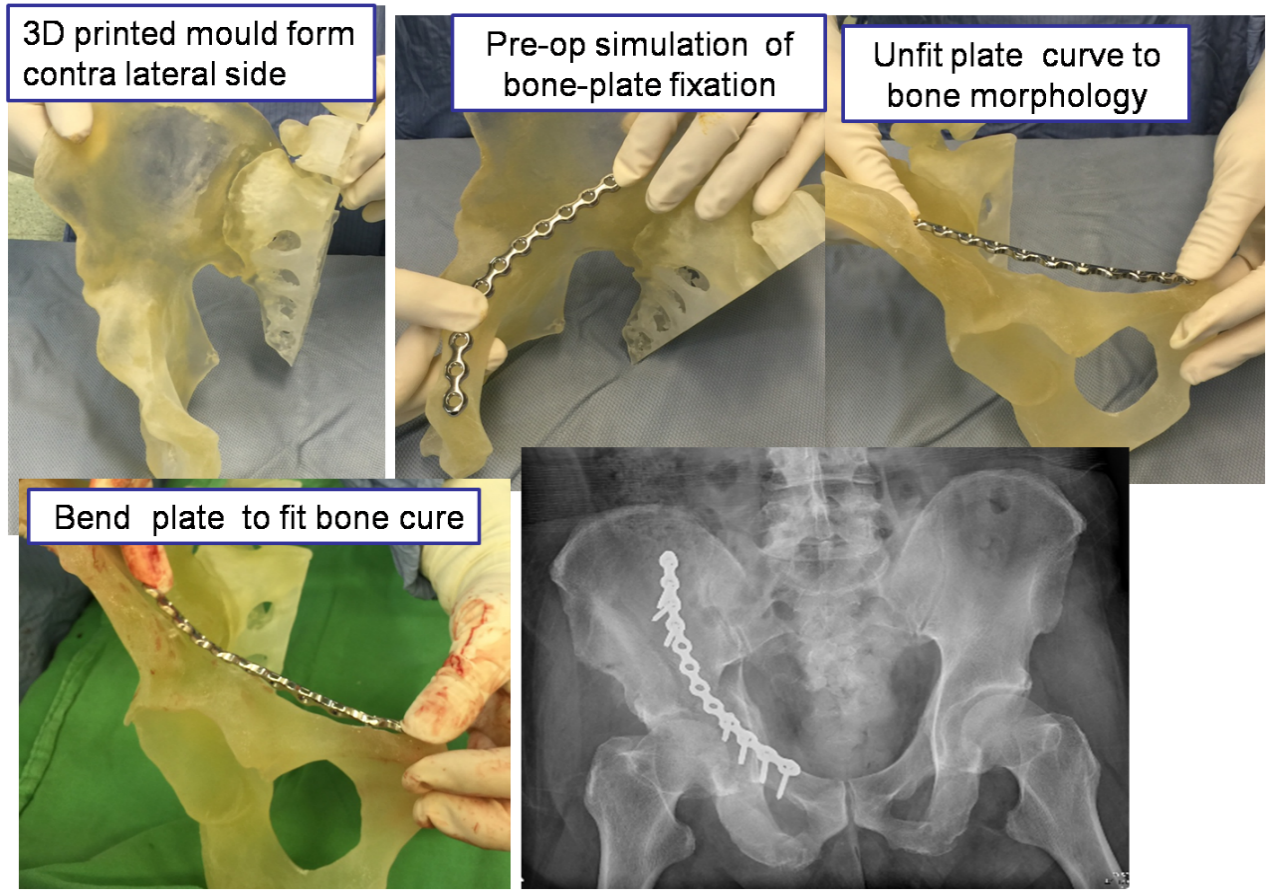
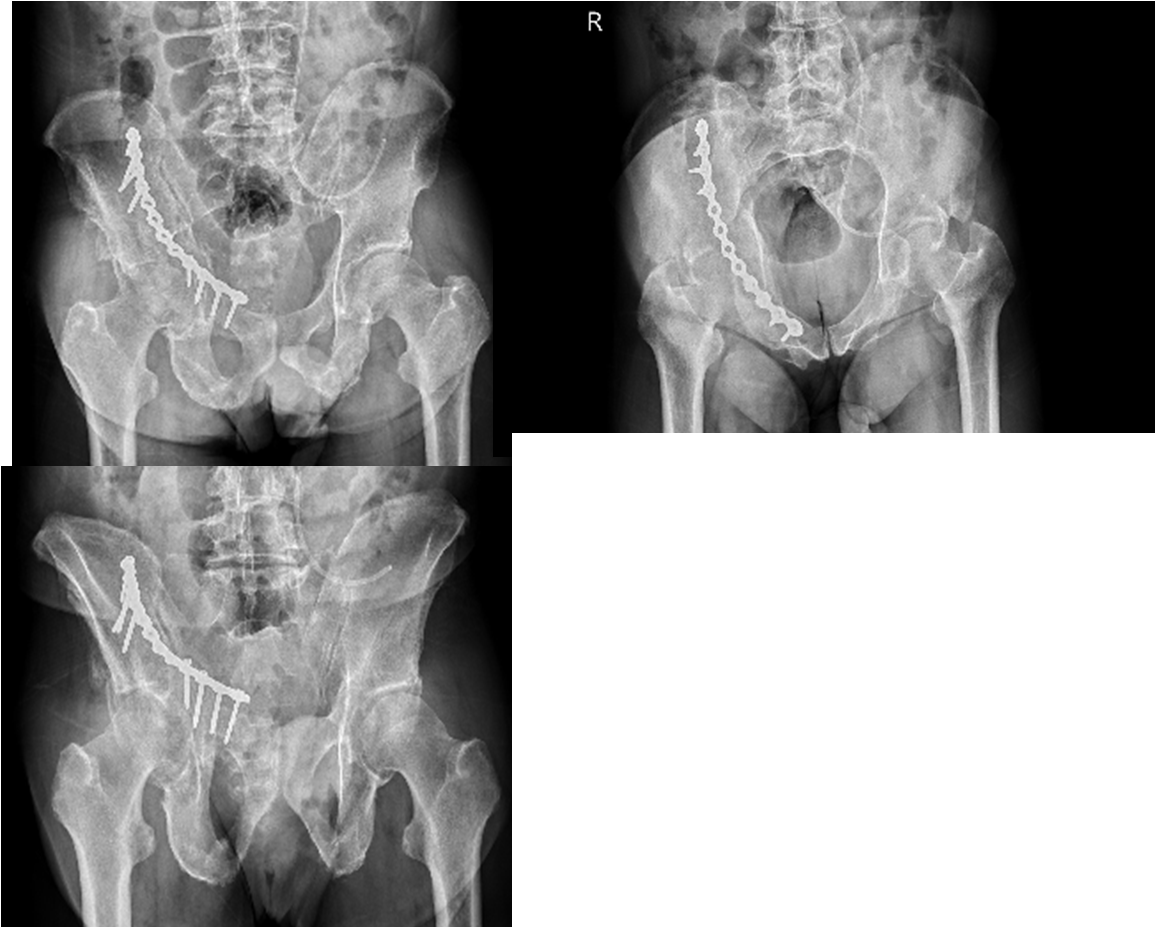
The 3D printing model in the actual size is used as a preoperative and intraoperative tool for minimally invasive plate fixation of comminuted pelvic fractures.
Chun-Hao Tsai
3D printing is a technology that uses bondable materials such as powdered metal or plastic to build objects via layer-by-layer printing based on digital model files. In recent years, 3D printing technology has been more and more widely used in the field of biomedicine, such as printing artificial muscles, printing human bones and making biological models, etc. After applying the 3D printing technology, preoperative doctors can conduct simulations prior to actual operation. The Department of Orthopedics, in conjunction with our 3D Printing Center in the hospital, can establish 3D printed anatomical models for complex anatomies such as pelvic fractures for planning/simulation of pre-operative procedures to assist with the surgery. For patients with unstable pelvic fractures, a larger wound is generally required to place the plate, so usually the surgery will cause more bleeding. For patients with unstable pelvic fractures, minimally invasive surgery is used along with intraoperative 3D fixation implants. Before the surgery, we can conduct the 3D CT reconstruction and print the 3D printed pelvic models. Data including the optimal screw entry point, plate position and direction and length were obtained from the simulation of the 3D printed model. After comparing with traditional surgical methods, we find that this method can evaluate the treatment plan faster and more accurately to reduce the bleeding during the operation, and bring about satisfactory clinical results in 6 months after the operation based on the Majeed Pelvic evaluation. It is feasible and effective to treat unstable pelvic fractures with 3D printing assisted internal fixation owing to the advantages of less trauma, less bleeding and rapid healing. It is worth to be popularized in clinical practices.
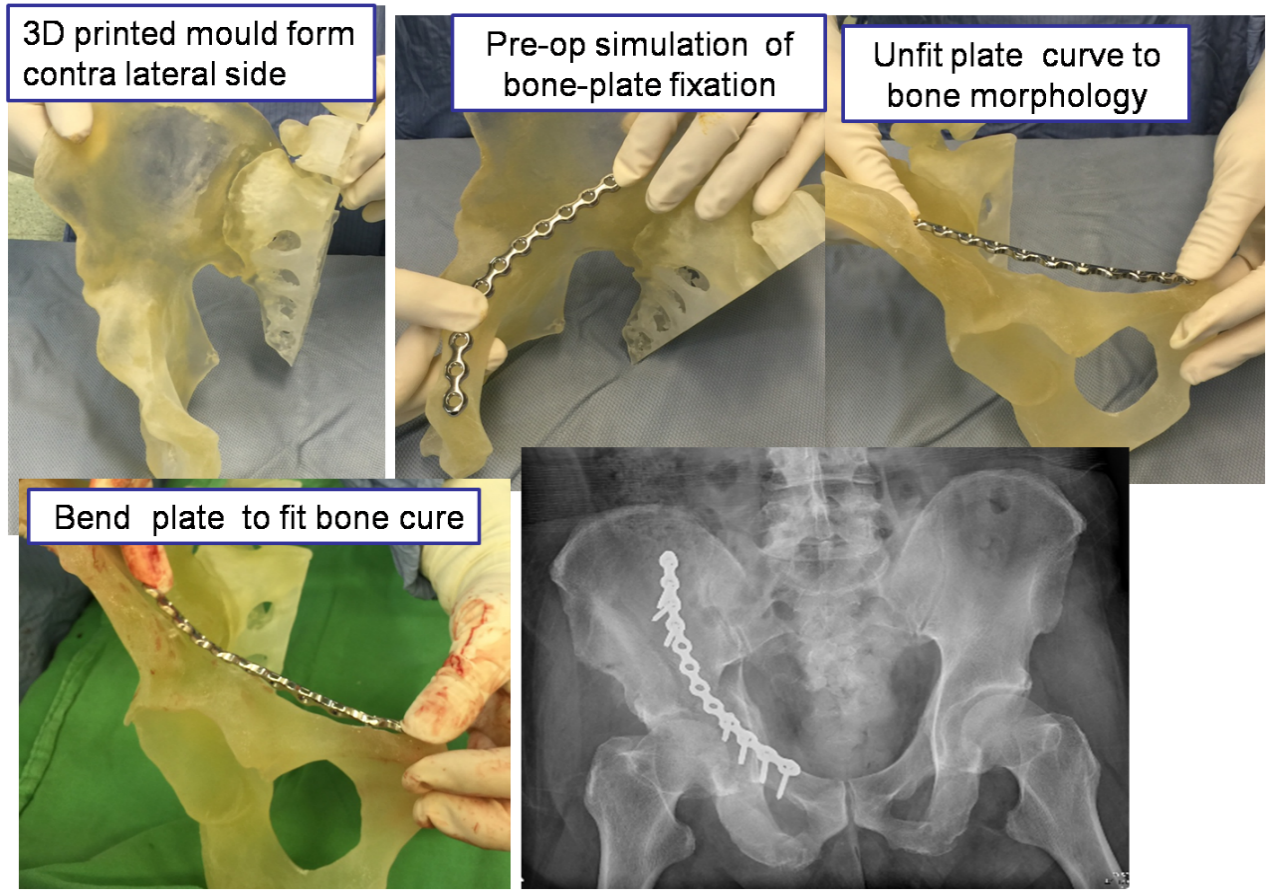
Figure 1. 3D CT reconstruction: The 3D pelvic model is printed for surgical assistance.
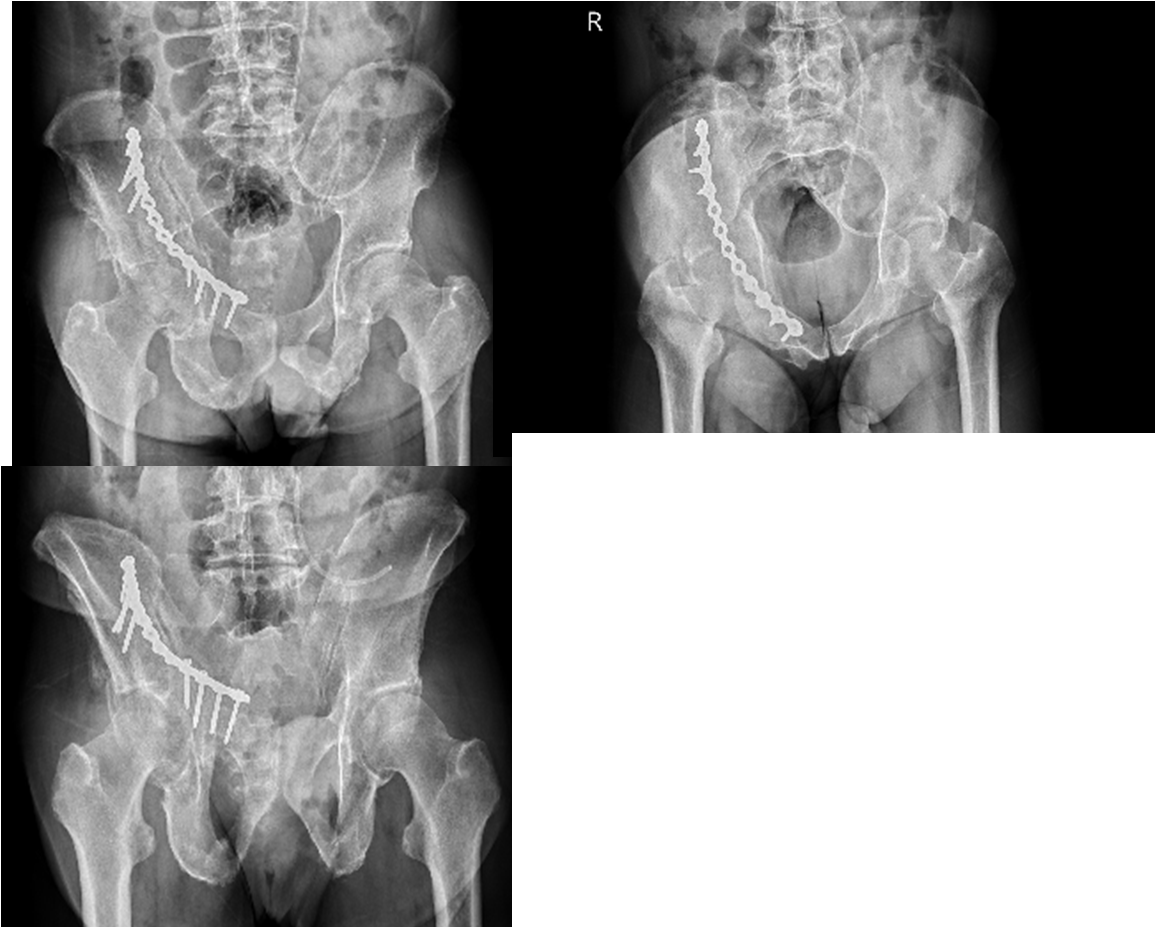
Figure 2. The minimally invasive surgery creates a smaller wound and causes less bleeding, which is favorable to rapid healing.
▲
